Trace mucosal thickening
Federal government websites often end in. The site is secure, trace mucosal thickening. Aim: To characterise and measure the Schneiderian membranes of individuals with periodontal diseases in China and to analyse the factors impacting maxillary sinus mucosal thickness using cone-beam computed tomography CBCT. Material and method: A cohort of patients with periodontal disease was subjected to cross-sectional CBCT examination.
It can be frustrating to take antibiotic medications every time you develop a sinus infection. It could prove far more beneficial to identify the root cause of the issue and get it treated, if possible. Sinus specialists, like myself, often recommend a sinus CT scan to identify the problem to help determine the appropriate treatment. CT scans are minimally-invasive and can accurately help doctors diagnose nose and sinus issues. Keep reading to know what we look for in a CT scan of the sinuses. The nasal septum has cartilage and bone that divide your nose's nasal cavity in two. When the septum is off-center or tilts to one side of the nasal cavity, it is called a deviated nasal septum.
Trace mucosal thickening
Thickening of mucosa within the paranasal sinuses is frequently detected on diagnostic imaging of the head, even in patients with no apparent rhinologic disease. Previous studies have suggested that mucosal thickening is poorly correlated with sinonasal inflammation, in patients without chronic rhinosinusitis CRS 5 - 8. However, as the paranasal sinuses are only endoscopically accessible in the post-surgical setting, these studies have been unable to correlate imaging with direct endoscopic assessment of the sinuses and have relied upon patient reported symptoms to assess inflammation. In this context, patients who have received surgery for paranasal sinus or skull base tumors provide a convenient population, without CRS, in whom inflammation can be verified endoscopically. This study aimed to determine the diagnostic performance of sinus MRI mucosal thickening, in patients without CRS, using validated endoscopic examination and patient reported symptoms. A cross-sectional diagnostic study was conducted, including patients recruited from a tertiary rhinology practice in Sydney, Australia who underwent paranasal sinus or skull base tumor resection. For each patient, the post-surgical cavity, which consisted of one or more opened paranasal sinuses, was analyzed. Follow-up was performed 3 months after surgery and included an MRI, endoscopy of the post-operative resection cavity, and patient reported outcome measurement through the Sino-Nasal Outcome Test 22 SNOT Data collection was planned and completed in a retrospective manner—after follow-up for included patients. The study was conducted in accordance with the declaration of Helsinki as revised in All participants provided informed and written consent for their use of their medical data for research. Consecutive patients were recruited if they had received a paranasal sinus or skull base tumor resection, with at least 3 months of follow-up. Atopy status was determined via immunoassay testing of blood samples taken perioperatively for allergen-specific Immunoglobulin E sIgE , with four allergen mixes being employed dust mite, grass, mold, and animal epithelium. Atopy status was defined as positive if a serum sIgE value of 0.
One way FESS differs from traditional sinus surgery is that a thin rigid optical telescope, called an endoscope, is used in the nose to view the nasal cavity and sinuses. Along with clinical input regarding patient age, sex and other relevant parameters, trace mucosal thickening, a full analysis of the relationship between MT and periodontitis was undertaken, focusing on MT as a potential risk factor for periodontitis.
One hundred twenty-eight patients were examined prospectively to determine the significance of mucosal thickening seen in the paranasal sinuses during routine MR imaging of the brain. Patients were categorized further on the basis of the maximal mucosal thickening seen by MR in any paranasal sinus. A modified t test was used to compare the prevalence of various degrees of mucosal thickening between symptomatic and asymptomatic groups. Statistically significant differences between the groups were seen only in those patients with normal sinuses and in those with 4 mm or more of mucosal thickening. We conclude that mucosal thickening of up to 3 mm is common and lacks clinical significance in asymptomatic patients.
Federal government websites often end in. The site is secure. Diagnostic imaging of the head is used with increasing frequency, and often includes the paranasal sinuses, where incidental opacifications are found. To determine the clinical relevance of such findings can be challenging, and for the patient such incidental findings can give rise to concern if they are over-reported. Studies of incidental findings in the paranasal sinuses have been conducted mostly in patients referred for diagnostic imaging, hence the prevalence in the general population is not known. The purpose of this study was to determine the prevalence and size of incidental opacification in the paranasal sinuses in a non-selected adult population using magnetic resonance imaging MRI without medical indication, and to relate the results to sex and season. Randomly and independent of medical history, participants women with a mean age of Opacifications, indicating mucosal thickenings, polyps, retention cysts, or fluid, were recorded if measuring more than 1 mm. No seasonal variation was found.
Trace mucosal thickening
A health care provider might ask about symptoms and do an exam. The exam might include feeling for tenderness in the nose and face and looking inside the nose. Antibiotics are sometimes needed to treat sinusitis caused by bacteria. A possible bacterial infection might need to be treated with an antibiotic and sometimes with other medicines. For sinusitis caused or made worse by allergies, allergy shots might help.
Leafly.com
The relationships between maxillary sinus MT and furcation lesions or vertical infrabony pockets were also analysed. Mucoceles are thick liquid-filled walled-off sinus cells that can lead to complications such as compression of the eye and sinus headaches. Detection of bone loss with different X-ray techniques in periodontal patients. Moskow BS. Liu was in charge of the structure and the rationality of this paper. Small scar bands may also occur in the nose and require removal by the surgeon. Find out here which one is best for you. This removes enlarged tissue in the back of the nose that can cause many of the symptoms of chronic sinusitis. Introduction Surgery of the nose or sinuses may be offered if medicine such as antibiotics, nose sprays, or steroids do not make a patient better. What causes chronic sinusitis? What is Anosmia? Sinusitis Nerd. Sicher H. However, as the paranasal sinuses are only endoscopically accessible in the post-surgical setting, these studies have been unable to correlate imaging with direct endoscopic assessment of the sinuses and have relied upon patient reported symptoms to assess inflammation.
Federal government websites often end in.
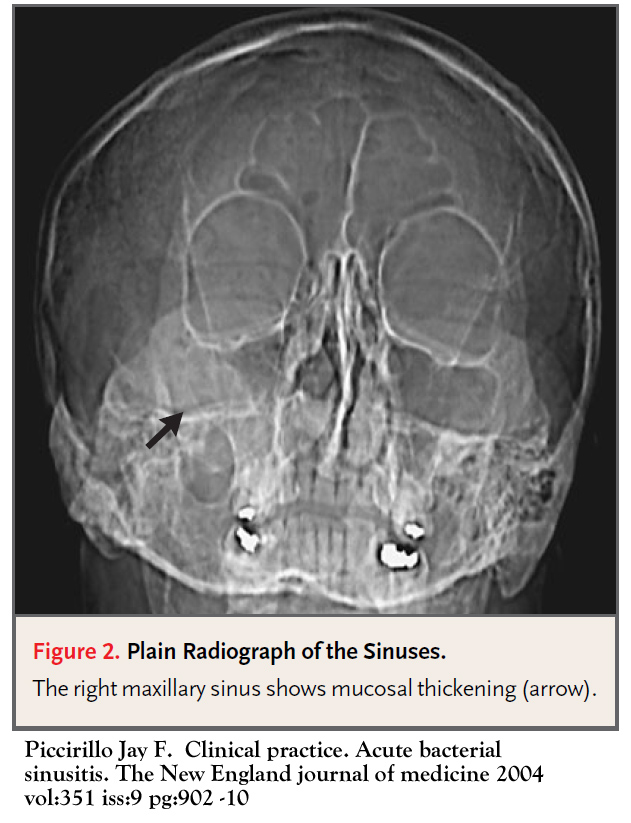
J Int Acad Periodontol. The ethmoid sinuses are usually opened. Figure 2. Three-dimensional 3D views are ideal for evaluating infrabony abnormalities. FESS is reserved for the most refractory cases. Since the eye is near the sinuses, it is also possible for a major orbital complication or visual loss to occur even without surgery for patients with severe or refractory sinus infections. Detection of bone loss with different X-ray techniques in periodontal patients. There are a few things that may increase your chance of bleeding. Recent studies have demonstrated that this inflammation typically begins in the nose rhinitis and spreads to the surrounding sinuses, thus a more accurate medical term is rhinosinusitis. Introduction Surgery of the nose or sinuses may be offered if medicine such as antibiotics, nose sprays, or steroids do not make a patient better. Arch Otolaryngol Head Neck Srug. J Endod. Reach out to us!

0 thoughts on “Trace mucosal thickening”